A series of three papers appeared this week in which we contributed towards therapeutic strategies in pancreatic cancer. A nice summary of results from our collaborative efforts ongoing for quite some years. That all those were accepted within one week we take as encouragement for our ongoing collaborations. Congrats to Alessandro, Cecilia, Ginevra & Stefano. Also thanks to our collaborators for the endeavor: Annarosa, Elisa and Erik.
“Integrins regulate hERG1 dynamics by girdin-dependent Gαi3: signaling and modeling in cancer cells.”
Duranti, C., J. Iorio, G. Bagni, G. C. Altadonna, T. Fillion, M. Lulli, F. N. D’Alessandro, A. Montalbano, E. Lastraioli, D. Fanelli, S. Coppola, T. Schmidt, F. Piazza, A. Becchetti and A. Arcangeli.
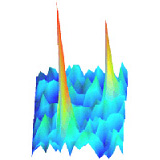
The hERG1 potassium channel is aberrantly over expressed in tumors and regulates the cancer cell response to integrin-dependent adhesion. We unravel a novel signaling pathway by which integrin engagement by the ECM protein fibronectin promotes hERG1 translocation to the plasma membrane and its association with β1 integrins, by activating girdin-dependent Gαi3 proteins and protein kinase B (Akt). By sequestering hERG1, β1 integrins make it avoid Rab5-mediated endocytosis, where unbound channels are degraded. The cycle of hERG1 expression determines the resting potential (Vrest) oscillations and drives the cortical f-actin dynamics and thus cell motility. To interpret the slow biphasic kinetics of hERG1/β1 integrin interplay, we developed a mathematical model based on a generic balanced inactivation–like module. Integrin-mediated cell adhesion triggers two contrary responses: a rapid stimulation of hERG1/β1 complex formation, followed by a slow inhibition which restores the initial condition. The protracted hERG1/β1 integrin cycle determines the slow time course and cyclic behavior of cell migration in cancer cells.
to be read in: Life Science Alliance (2023) 7:e202302135.
“Differential sensitivity to ionizing radiation in gemcitabine- and paclitaxel-resistant pancreatic cancer cells.”
Che, P. P., A. Gregori, C. Bergonzini, M. Ali, G. Mantini, T. Schmidt, F. Finamore, S. M. F. Rodrigues, A. E. Frampton, L. A. McDonnell, E. H. Danen, B. J. Slotman, P. Sminia and E. Giovannetti.
Chemoresistance remains a major challenge in treating pancreatic ductal adenocarcinoma (PDAC). While chemoradiation has proven effective in other tumor types, such as head-and-neck squamous cell carcinoma, its role in PDAC and its impact on acquired chemoresistance have yet to be fully explored. In this study, we investigated the sensitivity of gemcitabine- and paclitaxel-resistant PDAC cells to ionizing radiation (IR) and their underlying mechanisms. Gemcitabine-resistant (GR) and paclitaxel-resistant (PR) clones were generated from PANC-1, PATU-T and SUIT2-007 pancreatic cancer cell lines. Cell survival after radiation was assessed using clonogenic assay, SRB assay, apoptosis and spheroid growth by bioluminescence while radiation-induced DNA damage was evaluated with Western blot, XL-PCR, ROS production and immunofluorescence. Autophagy and modulation of Hippo pathway were investigated using proteomics, Western blot, immunofluorescence and RT-qPCR. In both 2D and 3D settings, PR cells were more sensitive to IR and showed decreased β-globin amplification indicating more DNA damage accumulation as compared to GR or wild-type (WT) cells after 24 hours. Proteomics analysis of PATU-T PR revealed that the protein MST4, a kinase involved in autophagy and Hippo signaling pathway, was highly downregulated. Differential association was found between autophagy and radiation treatment depending on the cell model. Interestingly, increased YAP nuclear localization and downstream Hippo pathway target gene expression were observed in in SUIT2-007 PR cells in response to IR, as compared to WT and GR. This is the first study investigating the potential of IR in targeting PDAC cells with acquired chemoresistance. Our results demonstrate that PR cells exhibit enhanced sensitivity to IR due to greater accumulation of DNA damage. Additionally, depending on the specific cellular context, radiation-induced modulation of autophagy and the Hippo pathway emerged as potential underlying mechanisms, and these findings have the potential to inform personalized treatment strategies for patients with acquired chemoresistance.
to be read in: J Rad Oncology (2023) nn:nnnn.
“ABCB1 overexpression through locus amplification represents an actionable target to combat paclitaxel resistance in pancreatic cancer cells.”
Cecilia Bergonzini, Alessandro Gregori, Tessa M.S. Hagens, Vera E. van der Noord, Bob van de Water, Annelien J.M. Zweemer, Mjriam Capula, Giulia Mantini, Asia Botto, Francesco Finamore, Ingrid Garajova, Liam A. McDonnell, Thomas Schmidt, Elisa Giovannetti, Erik H.J. Danen.
Chemotherapies such as gemcitabine/nab-paclitaxel are confronted with intrinsic or acquired resistance in pancreatic ductal adenocarcinoma (PDAC). We aimed to identify novel actionable mechanisms to overcome such resistance.Three paclitaxel (PR) and gemcitabine resistant (GR) PDAC models were established. Transcriptomics and proteomics were used to identify conserved mechanisms of drug resistance. Genetic and pharmacological approaches were used to overcome paclitaxel resistance. Upregulation of ABCB1 through locus amplification was identified as a conserved feature unique to PR cells. ABCB1 was not affected in any of the GR models and no cross resistance was observed. The ABCB1 inhibitor verapamil or siRNA mediated ABCB1 depletion sensitized PR cells to paclitaxel and prevented efflux of ABCB1 substrates in all models. ABCB1 expression was detected in PDAC patients that had received gemcitabine/nab-paclitaxel treatment. A pharmacological screen identified known and novel kinase inhibitors that attenuate efflux of ABCB1 substrates and sensitize PR PDAC cells to paclitaxel. Upregulation of ABCB1 through locus amplification represents a novel, conserved mechanism of PDAC paclitaxel resistance. ABCB1 has not been previously implicated in PR PDAC. The synthetic lethal interactions identified in this study can be further (pre)clinically explored as therapeutic strategies to overcome paclitaxel resistance in PDAC.
to be read in: J Exp & Clinical Cancer Res. (2023) nn:nnnn.